What's in this article?
What is Chronic Myeloid Leukemia?
Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer, and can spread to other areas of the body. To learn more about how cancers start and spread, see What is Cancer?
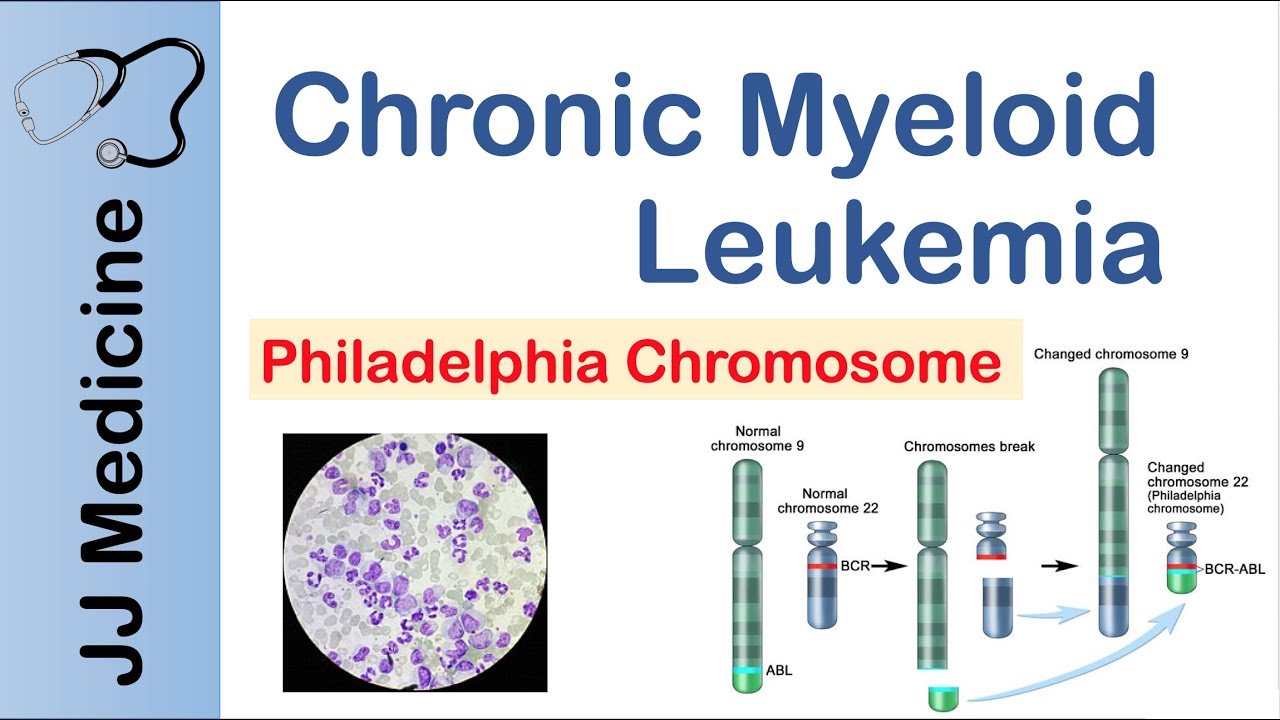
Chronic myeloid leukemia (CML), also known as chronic myelogenous leukemia, is a type of cancer that starts in certain blood-forming cells of the bone marrow. In CML, a genetic change takes place in an early (immature) version of myeloid cells – the cells that make red blood cells, platelets, and most types of white blood cells (except lymphocytes). This change forms an abnormal gene called BCR-ABL, which turns the cell into a CML cell. The leukemia cells grow and divide, building up in the bone marrow and spilling over into the blood. In time, the cells can also settle in other parts of the body, including the spleen. CML is a fairly slow growing leukemia, but it can also change into a fast-growing acute leukemia that is hard to treat.
Most cases of CML occur in adults, but very rarely it occurs in children, too. In general, their treatment is the same as for adults.
Signs and Symptoms of Chronic Myeloid Leukemia
The clinical manifestations of Chronic myeloid leukemia are insidious, changing somewhat as the disease progresses through its 3 phases (chronic, accelerated, and blast). Signs and symptoms in the chronic phase are as follows:
-
Fatigue, weight loss, loss of energy, decreased exercise tolerance
-
Low-grade fever and excessive sweating from hypermetabolism
-
Elevated white blood cell (WBC) count or splenomegaly on routine assessment
-
Early satiety and decreased food intake from encroachment on stomach by enlarged spleen
-
Left upper quadrant abdominal pain from spleen infarction
-
Hepatomegaly
The following are signs and symptoms of progressive disease:
-
Bleeding, petechiae, and ecchymoses during the acute phase
-
Bone pain and fever in the blast phase
-
Increasing anemia, thrombocytopenia, basophilia, and a rapidly enlarging spleen in blast crisis
Causes of Chronic Myeloid Leukemia
Most people will never know what caused them to get chronic myeloid leukemia. You don’t typically get it from your parents or from infections. Your smoking habits and diet don’t seem to raise your chance of getting it either.
The only known risk is if you’ve been in contact with high levels of radiation.
What are the other types of leukemia?
There are 4 main types of leukemia, based on whether they are acute or chronic, and myeloid or lymphocytic:
- Acute myeloid leukemia (AML)
- Chronic myeloid leukemia (CML)
- Acute lymphocytic leukemia (ALL)
- Chronic lymphocytic leukemia (CLL)
In acute leukemias, the bone marrow cells cannot mature the way they should. These immature cells continue to reproduce and build up. Without treatment, most people with acute leukemia would only live a few months. Some types of acute leukemia respond well to treatment, and many patients can be cured. Other types of acute leukemia have a less favorable outlook. Lymphocytic leukemias (also known as lymphoid or lymphoblastic leukemia) start in the cells that become lymphocytes. Lymphomas are also cancers that start in those cells. The main difference between lymphocytic leukemias and lymphomas is that in leukemia, the cancer cell is mainly in the bone marrow and blood, while in lymphoma it tends to be in lymph nodes and other tissues.
Chronic Myeloid Leukemia Diagnosis
Tests and procedures used to diagnose chronic myelogenous leukemia include:
- Physical exam. Your doctor will examine you and check such vital signs as pulse and blood pressure. He or she will also feel your lymph nodes, spleen and abdomen for abnormalities.
- Blood tests. A complete blood count may reveal abnormalities in your blood cells. Blood chemistry tests to measure organ function may also reveal abnormalities that can help your doctor make a diagnosis.
- Bone marrow tests. Bone marrow biopsy and bone marrow aspiration are used to collect bone marrow samples for laboratory testing. These tests involve collecting bone marrow from your hipbone.
- Tests to look for the Philadelphia chromosome. Specialized tests, such as fluorescence in situ hybridization (FISH) analysis and the polymerase chain reaction (PCR) test, analyze blood or bone marrow samples for the presence of the Philadelphia chromosome or the BCR-ABL gene.
Phases of chronic myelogenous leukemia
The phase of chronic myelogenous leukemia refers to the aggressiveness of the disease. Your doctor determines the phase by measuring the proportion of diseased cells to healthy cells in your blood or bone marrow. A higher proportion of diseased cells means chronic myelogenous leukemia is at a more advanced stage.
Phases of chronic myelogenous leukemia include:
- Chronic. The chronic phase is the earliest phase and generally has the best response to treatment.
- Accelerated. The accelerated phase is a transitional phase when the disease becomes more aggressive.
- Blastic. Blastic phase is a severe, aggressive phase that becomes life-threatening.
Chronic Myeloid Leukemia Treatment
The goal of your treatment is to destroy the leukemia blood cells in your body and restore healthy ones to a normal level. It’s usually not possible to get rid of all the bad cells.
If you get treatment during the early, chronic phase of chronic myelogenous leukemia, it can help prevent the disease from moving to a more serious level.
Doctors usually give drugs known as tyrosine kinase inhibitors (TKIs) first. They slow down the rate at which your body makes leukemia cells.
Some TKIs that are commonly used include:
- Dasatinib (Sprycel)
- Imatinib (Gleevec)
- Nilotinib (Tasigna)
You may get bosutinib (Bosulif) and ponatinib (Iclusig) if other drugs don’t help or make you too sick.
If your disease continues to get worse after you’ve used two or more TKIs, your doctor may suggest a drug called omacetaxine mepesuccinate (Synribo).
Other CML treatment options include chemotherapy and biologic therapy, which uses a medication called interferon to help stir up action in your immune system your body’s defense against germs.
A stem cell transplant might cure some patients. It’s a complicated procedure that’s usually done only when your other treatments aren’t working. Stem cells are in the news a lot, but usually when you hear about them they’re referring to “embryo” stem cells that are used in cloning. The stem cells in a stem cell transplant are different. These are cells that live in your bone marrow and help make new blood cells.
When you get a stem cell transplant, a donor will supply the new stem cells. You’ll need to get on a waiting list to find a donor who is the right match you so that your body doesn’t “reject” them.
Close relatives, such as your brother or sister, are the best chances for a good match. If that doesn’t work out, you need to get on a list of potential donors from strangers. Sometimes the best odds for the right stem cells for you will be from someone who is in the same racial or ethnic group as you.




Leave a Comment