What's in this article?
What is Essential Thrombocythemia?
Essential Thrombocythemia (ET) is a chronic myeloproliferative neoplasm characterized by an increased number of platelets in the circulating blood. The disease is commonly diagnosed at the age of 60, predominately in women. ET is characterized by a proliferation of platelet precursors in the bone marrow, and its most common complications include tendencies toward blood clotting and/or bleeding; later but more rare consequences include a transformation to myelofibrosis (marrow scarring) or acute leukemia.
Symptoms of Essential Thrombocythemia
The greatest health risk in patients with ET is an increased risk of developing blood clots. Blood clots can be in the deep vessels of the legs or lungs; ET patients are also more likely to experience strokes and heart attacks. ET patients can develop clots elsewhere, including within the abdomen, an otherwise rare site for clots to form. The risk of clotting increases with age, and disease-associated risks may be quite different for children than for adults, with children generally being at low risk for clots and other problems related to ET. In addition (and somewhat counter-intuitively) a subset of ET patients may also be more likely to bleed; this appears to be restricted to a small minority of patients with a very high (over 1.5 million) platelet count. Other symptoms in ET include headaches, fatigue, temporary changes in vision, dizziness, ringing in the ears, vertigo and tingling in the hands.
Very rarely, patients with ET can experience an evolution from ET to a more advanced blood disease. ET can evolve into a related disease called myelofibrosis, or into acute leukemia. This evolution is sufficiently rare (within what is already a rare disease), that the estimates of the risk are imprecise but are thought to be on the order of 1-2% of patients with ET over a lifetime.
How do people inherit Essential Thrombocythemia?
Most cases of essential thrombocythemia are not inherited. Instead, the condition arises from gene mutations that occur in early blood-forming cells after conception. These alterations are called somatic mutations.
Less commonly, essential thrombocythemia is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. When it is inherited, the condition is called familial essential thrombocythemia.
How is Thrombocytosis Diagnosed?
Finding the underlying condition (such as iron deficiency anemia, cancer, or infection) can aid in the diagnosis and management of thrombocytosis. If no secondary cause is identified, the patient is presumed to have ET. A blood test for a specific gene, called JAK2, is diagnostic of the disorder, but positive in only about 50% of the cases. The patient may have to undergo bone marrow aspiration (removal and examination of bone marrow) and other blood tests to confirm the diagnosis.
Causes of Essential Thrombocythemia?
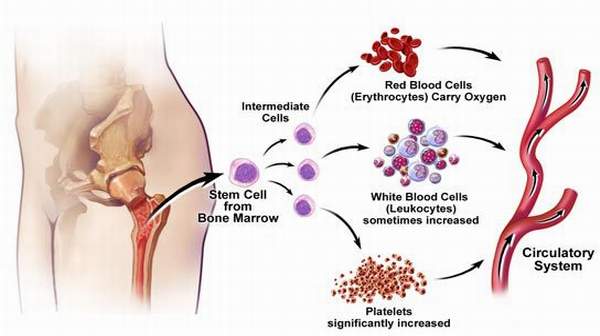
Bone marrow spongy tissue inside your bones contains stem cells that can become red blood cells, white blood cells or platelets (thrombocytes). Platelets stick together, helping blood to form a clot that stops bleeding when you damage a blood vessel, such as when you get a cut. A normal platelet count ranges from 150,000 to 450,000 platelets per microliter of blood.
If you have essential, or primary, thrombocythemia, your bone marrow makes too many platelet-forming cells (megakaryocytes). The excess platelets may not function normally, leading to abnormal clotting or bleeding.
The exact cause of essential thrombocythemia and similar conditions, known as myeloproliferative disorders, isn’t known. About 80 percent of people with the disorder have an acquired gene mutation contributing to the disease. This may involve the Janus kinase 2 (JAK2), calreticulin (CALR) or MPL gene mutation.
A high platelet count that’s caused by an underlying condition such as an infection or iron deficiency is called reactive, or secondary, thrombocythemia. People with secondary thrombocythemia have less risk of blood clots and bleeding than do people with essential thrombocythemia.
How is Thrombocytosis Treated?
Patients who have no symptoms may remain stable and only require routine check-ups by their physician. For those with symptoms, a few treatment options are available. One is to treat the disease that is causing thrombocytosis. In some cases, the patient can take aspirin to help prevent blood clots. The low dose used for this purpose does not usually cause stomach upset or bleeding.
In essential thrombocythemia, medications such as hydroxyurea or anagrelide are used to suppress platelet production by the bone marrow. These medications usually have to be taken indefinitely. In cases of severe life-threatening thrombocytosis, a procedure called plateletpheresis is performed to immediately lower the platelet count to safer levels. In this procedure, a special instrument is used to remove blood from the patient, separate and remove the platelets, and then return the other blood cells to the patient.