What's in this article?
What is Kidney Stones?
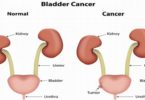
A kidney stone is a hard, crystalline mineral material formed within the kidney or urinary tract. Kidney stones are a common cause of blood in the urine (hematuria) and often severe pain in the abdomen, flank, or groin. Kidney stones are sometimes called renal calculi.
The condition of having kidney stones is termed nephrolithiasis. Having stones at any location in the urinary tract is referred to as urolithiasis, and the term ureterolithiasis is used to refer to stones located in the ureters.
Symptoms of Kidney Stones
A kidney stone may not cause symptoms until it moves around within your kidney or passes into your ureter the tube connecting the kidney and bladder. At that point, you may experience these signs and symptoms:
- Severe pain in the side and back, below the ribs
- Pain that radiates to the lower abdomen and groin
- Pain that comes in waves and fluctuates in intensity
- Pain on urination
- Pink, red or brown urine
- Cloudy or foul-smelling urine
- Nausea and vomiting
- Persistent need to urinate
- Urinating more often than usual
- Fever and chills if an infection is present
- Urinating small amounts
Pain caused by a kidney stone may change for instance, shifting to a different location or increasing in intensity as the stone moves through your urinary tract.
Causes of Kidney Stones
There is no consensus as to why kidney stones form.
- Heredity: Some people are more susceptible to forming kidney stones, and heredity may play a role. The majority of kidney stones are made of calcium, and hypercalciuria (high levels of calcium in the urine) is one risk factor. The predisposition to high levels of calcium in the urine may be passed on from generation to generation. Some rare hereditary diseases also predispose some people to form kidney stones. Examples include people with renal tubular acidosis and people with problems metabolizing a variety of chemicals including cystine (an amino acid), oxalate, (a salt of an organic acid), and uric acid (as in gout).
- Geographical location: There may be a geographic predisposition to forming kidney stones, so where a person lives may make it more likely for them to form kidney stones. There are regional “stone belts,” with people living in the southern United States having an increased risk of stone formation. The hot climate in this region combined with inadequate fluid intake may cause people to be relatively dehydrated, with their urine becoming more concentrated and allowing chemicals to come in closer contact to form the nidus, or beginning, of a stone.
- Diet: Diet may or may not be an issue. If a person is susceptible to forming stones, then foods high in animal proteins and salt may increase the risk; however, if a person isn’t susceptible to forming stones, diet probably will not change that risk.
Medications: People taking diuretics (or “water pills”) and those who consume excess calcium-containing antacids can increase the amount of calcium in their urine and potentially increase their risk of forming stones. Taking excess amounts of vitamins A and D are also associated with higher levels of calcium in the urine. Patients with HIV who take the medication indinavir (Crixivan) may form indinavir stones. Other commonly prescribed medications associated with stone formation include phenytoin (Dilantin) and antibiotics like ceftriaxone (Rocephin) and ciprofloxacin (Cipro). - Underlying illnesses: Some chronic illnesses are associated with kidney stone formation, including cystic fibrosis, renal tubular acidosis, and inflammatory bowel disease.
Who gets kidney stones?
Kidney stones are more common among males than females. Most people who experience kidney stones do so between the ages of 30 and 50. A family history of kidney stones also increases one’s chances of developing them.
Similarly, a previous kidney stone occurrence increases the risk that a person will develop subsequent stones in the future if preventative action is not taken.
Certain medications can increase the risk of developing kidney stones. Scientists found that topiramate (Topamax), a drug commonly prescribed to treat seizures and migraine headaches, can increase the likelihood of kidney stones developing.
Additionally, it is possible that long-term use of vitamin D and calcium supplements cause high calcium levels, which can contribute to kidney stones.
Additional risk factors for kidney stones include diets that are high in protein and sodium but low in calcium, a sedentary lifestyle, obesity, high blood pressure, and conditions that affect how calcium is absorbed in the body such as gastric bypass surgery, inflammatory bowel disease, and chronic diarrhea.
Treating kidney stones
Most kidney stones are small enough (less than 4mm in diameter) to be passed out in your urine and can probably be treated at home.
But even small kidney stones can be painful, although this usually only lasts a couple of days and disappears when the stone has been passed.
Medication
If you are in severe pain, your GP can give you pain relief by injection. A second dose can be given after half an hour if you’re still experiencing pain.
Medication can also be injected to treat the symptoms of nausea (feeling sick) and vomiting. This is called an anti-emetic (anti-sickness) medication.
You may also be given a prescription for painkillers, anti-emetics, or both, to take at home.
Self care
You may be advised to wait until you pass your kidney stone when you go to the toilet, and to try to collect it from your urine. You can do this by filtering your urine through gauze or a stocking.
Give the stone to your GP so that they can have it analysed to help determine any further treatment you may need.
You should drink enough water to make your urine colourless. If your urine is yellow or brown, you’re not drinking enough.



Leave a Comment