What's in this article?
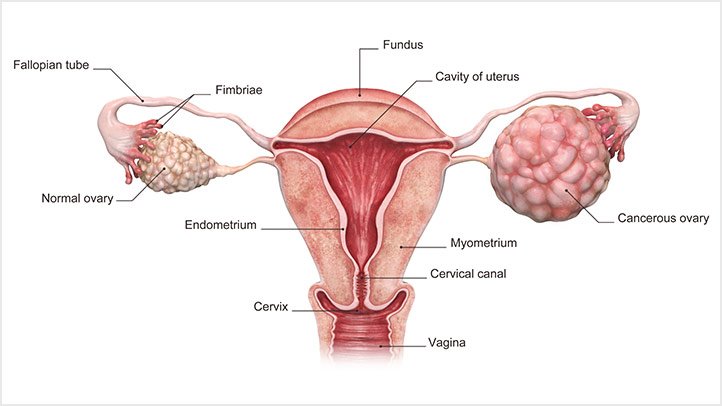
Ovarian cancer is a type of cancer that begins in the ovaries. Women have two ovaries, one on each side of the uterus. The ovaries each about the size of an almond produce eggs (ova) as well as the hormones estrogen and progesterone.
Ovarian cancer often goes undetected until it has spread within the pelvis and abdomen. At this late stage, ovarian cancer is more difficult to treat and is frequently fatal. Early-stage ovarian cancer, in which the disease is confined to the ovary, is more likely to be treated successfully.
Surgery and chemotherapy are generally used to treat ovarian cancer.
Symptoms of ovarian cancer
In the early stages, ovarian cancer usually has few symptoms; in many cases, there are no symptoms at all.
Patients often attribute their symptoms to other conditions, such as premenstrual syndrome,irritable bowel syndrome, or a temporary bladder problem.
The main difference between ovarian cancer and other possible disorders is the persistence and gradual worsening of symptoms.
The following are examples of possible early symptoms of ovarian cancer:
- Pain in the pelvis
- Pain on the lower side of the body
- Pain in the lower stomach
- Back pain
- Indigestion or heartburn
- Feeling full rapidly when eating
- More frequent and urgent urination
- Pain during sexual intercourse
- Changes in bowel habits, such as constipation
As ovarian cancer progresses, these symptoms are also possible:
- Nausea
- Weight loss
- Breathlessness
- Tiredness
- Loss of appetite
If an individual experiences bloating, pressure, or pain in the abdomen or pelvis that persists for more than a few weeks they should see a doctor immediately
What are ovarian cancer risk factors?
Risk factors are related to two major categories: menstrual cycles (ovulation) and family history. The more a woman ovulates (cycles) over her lifetime, the higher her risk of ovarian cancer. Thus starting her period (menarche) at a younger age, ending her period (menopause) at a late age, and never getting pregnant (nulliparity) are all risk factors. It was once thought that infertility patients who underwent preparation for IVF (ovarian stimulation for in vitro fertilization) were at increased risk, but this has since been shown not to be the case in a large comprehensive review of the subject.
Approximately 15% of ovarian cancers are genetically related. Because of this, current guidelines suggest that all women with ovarian cancer should undergo testing for BRCA1 and BRCA2 gene changes (mutations). All patients with ovarian cancer will ideally discuss this topic with their doctor. These gene mutations can affect males as well as females. If a patient is positive for one of these, then her siblings and her children can be tested as well.
Testing involves a simple blood test that can be drawn at many offices and laboratories. The results of this test can greatly affect how family members are monitored for various cancers, and family members of both sexes are encouraged to be tested.
When compared with the general population risk (1.3% of women will develop ovarian cancer), women with BRCA1 and BRCA2 genetic mutations have a 39% (BRCA1) or 11% to 17% (BRCA2) chance of developing ovarian cancer in their lifetime. Lynch syndrome (typically colon and uterine cancer), Li-Fraumeni syndrome, and Cowden’s syndrome are also associated with ovarian cancer but are less common.
The less common varieties of ovarian cancer (borderline, germ cell, and stromal tumors) have few definable risk factors. The germ cell tumors often seen at younger ages and are treated very differently both surgically and chemotherapeutically.
Causes of ovarian cancer
Several possible causes of ovarian cancer have been identified, along with risks that may make developing the condition more likely.
Cancer begins with a change (mutation) in the structure of the DNA in cells, which can affect how they grow. This means that cells grow and reproduce uncontrollably, producing a lump of tissue called a tumour.
In ovarian cancer, cells in the ovary start to change and grow abnormally. If the cancer isn’t identified at an early stage, it can spread to the abdomen and pelvis, including other parts of the female reproductive system.
Increased risk
The exact cause of epithelial ovarian cancer (the main type) isn’t known, but certain things may increase your risk of developing it.
Age
Your risk of ovarian cancer increases with age, with most cases occurring after the menopause. More than 8 out of 10 cases of ovarian cancer occur in women who are over 50 years of age.
Family history
If you have two or more close relatives (mother, sister or daughter) who developed ovarian cancer or breast cancer, your risk of also developing the condition may be increased.
If your relatives developed cancer before the age of 50, it’s more likely it was the result of an inherited faulty gene. BRCA1 and BRCA2 are faulty genes that are linked to ovarian cancer. They’re also known to increase the risk of breast cancer.
Having relatives with ovarian cancer doesn’t mean you definitely have a faulty gene in the family the cancer could have happened by chance. Only 1 in 10 (10%) of ovarian cancers are thought to be caused by a faulty gene.
You may be at a high risk of having a faulty gene if you have:
- one relative diagnosed with ovarian cancer at any age and at least two close relatives with breast cancer whose average age is under 60; all of these relatives should be on the same side of your family (either your mother’s OR father’s side)
- one relative diagnosed with ovarian cancer at any age and at least one close relative diagnosed with breast cancer under the age of 50; both of these relatives should come from the same side of your family
- two relatives from the same side of the family diagnosed with ovarian cancer at any age
If you’re at a higher risk of having a faulty gene, your GP can refer you for tests to check for faulty BRCA1 and BRCA2 genes.
Ovulation and fertility
Every time an egg is released into the reproductive system, the surface of the ovary breaks to let it out. The surface of the ovary is damaged during this process and needs to be repaired. Each time this happens, there’s a greater chance of abnormal cell growth during the repair.
This may be why the risk of ovarian cancer decreases if you take the contraceptive pill, or have multiple pregnancies or periods of breastfeeding. At these times, eggs aren’t released.
There’s no strong evidence to show that women who have infertility treatment have an increased risk of developing ovarian cancer. However, it’s thought that infertility itself may increase ovarian cancer risk and research into this area is being carried out.
Hormone replacement therapy (HRT)
Women who take hormone replacement therapy (HRT) have been shown to have a small increased risk of developing ovarian cancer. However, if HRT is stopped, after five years the risk is reduced to the same level as women who’ve never taken HRT.
Endometriosis
Endometriosis may also increase your risk of ovarian cancer. In endometriosis, the cells that usually line the womb grow elsewhere in the body.
These endometrial cells behave as if they were in the womb, so thickening and bleeding that usually occurs during menstruation occurs in other parts of the body. There’s no way for this endometrial tissue to leave the body so it becomes trapped, leading to pain, swelling and bleeding in that area.
Ovarian cancer Treatment
Types of treatment
The choice of treatment and the long-term outcome (prognosis) for women who have ovarian cancer depends on the type and stage of cancer. Your age, overall health, quality of life, and desire to have children must also be considered.
The main treatment choices are:
- Surgery to find out if you have cancer and to treat it. This may include taking biopsies to check for the spread of cancer.
- Chemotherapy , which uses medicines to kill cancer cells. It is recommended after surgery for most stages of ovarian cancer.
Women with more advanced ovarian cancer may have part of their chemotherapy before surgery and the rest of it after surgery. This can make the surgery safer for these women.
Radiation therapy may be used to destroy cancer cells using high-dose X-rays or other high-energy rays.
Side effects of treatment
Most treatments for ovarian cancer cause side effects. They may differ, depending on the type of treatment and your age and overall health.
- Side effects of surgery depend on the extent of your surgery. If the doctor removes your ovaries, you will no longer be able to bear children. And if you were still menstruating before your surgery, you will start menopause.
- Side effects of chemotherapy may include loss of appetite,nausea, vomiting, fatigue, and hair loss. There is also an increased chance of getting a serious infection.
Radiation treatment also can cause side effects.
Home treatment may help you manage the side effects.
Advanced-stage ovarian cancer
Surgery in advanced-stage ovarian cancer involves removing as much of the cancer as possible. The uterus, the tissue lining the abdominal wall (omentum), and any areas of visible cancer are removed. This may include surgery on the intestines, urinary system, or spleen, or scraping of the diaphragm to remove all the cancer. The long-term outcome is better if no cancer cells remain.
Coping with emotions
When you first find out that you have cancer, you may feel scared or angry. Or you may feel very calm. It’s normal to have a wide range of feelings and for those feelings to change quickly. Some people find that it helps to talk about their feelings with family and friends.
If your emotional reaction to cancer gets in the way of your ability to make decisions about your health, it’s important to talk with your doctor. Your cancer treatment center may offer psychological or financial services. And a local chapter of the American Cancer Society can help you find a support group.
Body image and sexual problems
Your feelings about your body may change after treatment for cancer. Managing body image issues may involve talking about your concerns with your partner and discussing your feelings with your doctor. Your doctor may also be able to refer you to groups that can offer support and information.
Palliative care
Palliative care is a kind of care for people who have a serious illness. It’s different from care to cure your illness. Its goal is to improve your quality of life-not just in your body but also in your mind and spirit.
You can have this care along with treatment to cure your illness.
Palliative care providers will work to help control pain or side effects. They may help you decide what treatment you want or don’t want. And they can help your loved ones understand how to support you.
If you’re interested in palliative care, talk to your doctor.
End-of-life care
For some people who have advanced cancer, a time comes when treatment to cure the cancer no longer seems like a good choice. This can be because the side effects, time, and costs of treatment are greater than the promise of cure or relief. But you can still get treatment to make you as comfortable as possible during the time you have left. You and your doctor can decide when you may be ready for hospice care.