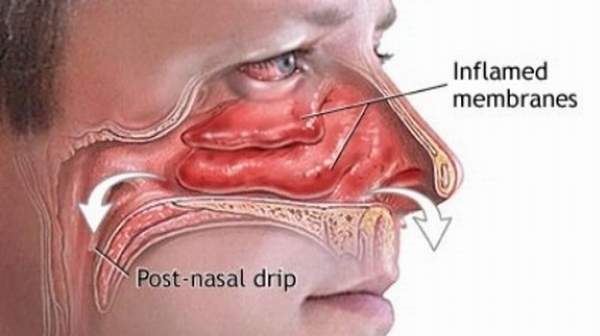
Postnasal drip, also termed upper airway cough syndrome, occurs when excess mucus accumulates in the back of the throat and creates the feeling of dripping mucus. Every day, glands in the lining of your nose, throat, airways, stomach, and intestinal tract produce about 1 to 2 quarts of mucus – a thick, wet substance that moistens these areas and helps trap and destroy foreign invaders like bacteria and viruses before they can get into your body and cause infection. Excess mucus can come out the front of your nose in the form of a runny nose. When the mucus runs down the back of the nose to the throat, it’s called postnasal drip.
Causes
There are a number of reasons that the glands in the nose may produce excess mucus such as:
- Colds and flu
- Sinus infections or sinusitis (an inflammation of the sinus)
- Allergies such as a reaction to pollen, animals and dust mites
- An object stuck in the nose (usually in a child)
- Pregnancy
- Medications (such as blood pressure medicines and contraceptive pills)
- A deviated septum (a problem with the wall between the two nostrils), nasal polyp (a fleshy swelling inside the nose) or other physical problem within the nose
- Cold temperatures, excess dryness or change in weather patterns
- Spicy foods and other food triggers
- Fumes produced by cleaning products, perfumes, smoke and other chemicals and irritants
Symptoms
Individuals may be diagnosed as suffering from post-nasal drip if they suffer from the following symptoms:
- Coughing
- Wheezing
- Constant swallowing, which can lead to an excessive amount of air in the stomach, causing discomfort
- Rhinorrhea, running nose due to mucus flow
- Frequent spitting
- Tickling in the throat
- Constant clearing of throat;
- Rigid burning sensation at back of the throat
- Broken or cracking voice, hoarseness
- Mucus feeling in the back of the throat
- Difficulty in breathing
- Congestion in the nasal and sinus passages
- Chronic sore throat
- Masses formed in the crypts of the tonsils that are generally yellow or white (commonly called tonsil stones, or tonsilloliths)
- Halitosis (bad breath)
- Snorting to clear mucus from the nasal passage that cannot otherwise be cleared by blowing one’s nose
- Cobblestone appearance of the oropharyngeal mucosa
- Frontal cranial pressure
- Fatigue
- Nausea
- Vomiting
Treatment
Treatment will depend on the cause. Often a postnasal drip will clear up by itself. If a viral infection or sinusitis is involved, antihistamines and decongestants may be useful, though decongestants are only for short-term relief. These can also be useful for treating postnasal drip associated with allergies, along with nasal sprays and steroid medications.
Other methods you can try include:
- Taking a mucus-thinning medication such as guaifenesin (Mucinex)
- Using saline nasal sprays or nasal irrigation (such as a neti pot) to flush excess mucus, bacteria, allergens, and other irritating substances out of the sinuses
- Turning on a vaporizer or humidifier to increase the moisture in the air
Try propping up your pillows at night so that the mucus doesn’t pool or collect in the back of your throat. If you have allergies, ways to reduce your triggers include:
- Covering your mattresses and pillowcases with dust-proof covers
- Washing all sheets, pillowcases, and mattress covers often in hot water
- Using special HEPA air filters in your home
- Dusting and vacuuming regularly
Call your doctor if the nasal drainage is foul smelling, you have a fever, you’re wheezing, or your symptoms last for 10 days or more, because you might have a bacterial infection. Let your doctor know right away if you notice blood in your postnasal drip. If medication isn’t helping your postnasal drip, you might need to see an otolaryngologist for evaluation, which can include a CT scan, X-rays, or other tests.